HEALTH MINDED . . . SAPPHIRE YEAR FOR PEOPLES' SELF-HELP HOUSING by Bonnie Carroll 
Sapphire Dinner & Live Auction The 45th Anniversary (Sapphire Anniversary) Central Coast Taste of hope Dinner celebrating Peoples' Self-Help Housing was held in November at the Santa Barbara Historical Museum, where guests honored the organization who developed over 1,600 rented units that house more than 5,000 low-income residents. PSHH also assisted nearly 1,200 low-income Self-Help Home Builders build and own their own first home.  .JPG)
Rochelle Rose PSHHC(Center) with Media VIPs KEYT3 Meredith Garofalo & MC Andrew Firestone “It has been an amazing 45 years. We have been pushed by the critical need for housing tht we see in our communities every day,” said President/CEO John Fowler. “We welcome and thank who have helped shelter so many working families in safe affordable homes to enjoy the Sapphire dinner.”  .jpg) 
Grassini Family Vinyards "Sapphire Cocktail" Island Brewing Co. The cocktail hour featured pours from local vintners Grassini Family Vinyards and Sanger Family of Wines, Marianello, and Tre Anelli, with beer from Island Brewing Company. A delicious blue sapphire cocktail was also being served to enjoy with appetizers of Shrimp Newburg in Pastry Shells and Stuffed Deviled Eggs. Following awards presented by PSHH President & CEO John Fowler and Master of Ceremonies Andrew Firestone, businessman and TV personality, a video on the work done by PSHH led into a silent auction that raised nearly $130,000 to support the charity. The outstanding dinner was prepared by star chef Michael Hutchings and his staff, and included Supreme of Chicken Tarragon Jus with Wild Rice Pilaf paired with Fess Parker wine, and was followed with an amazing logo birthday cake dessert. 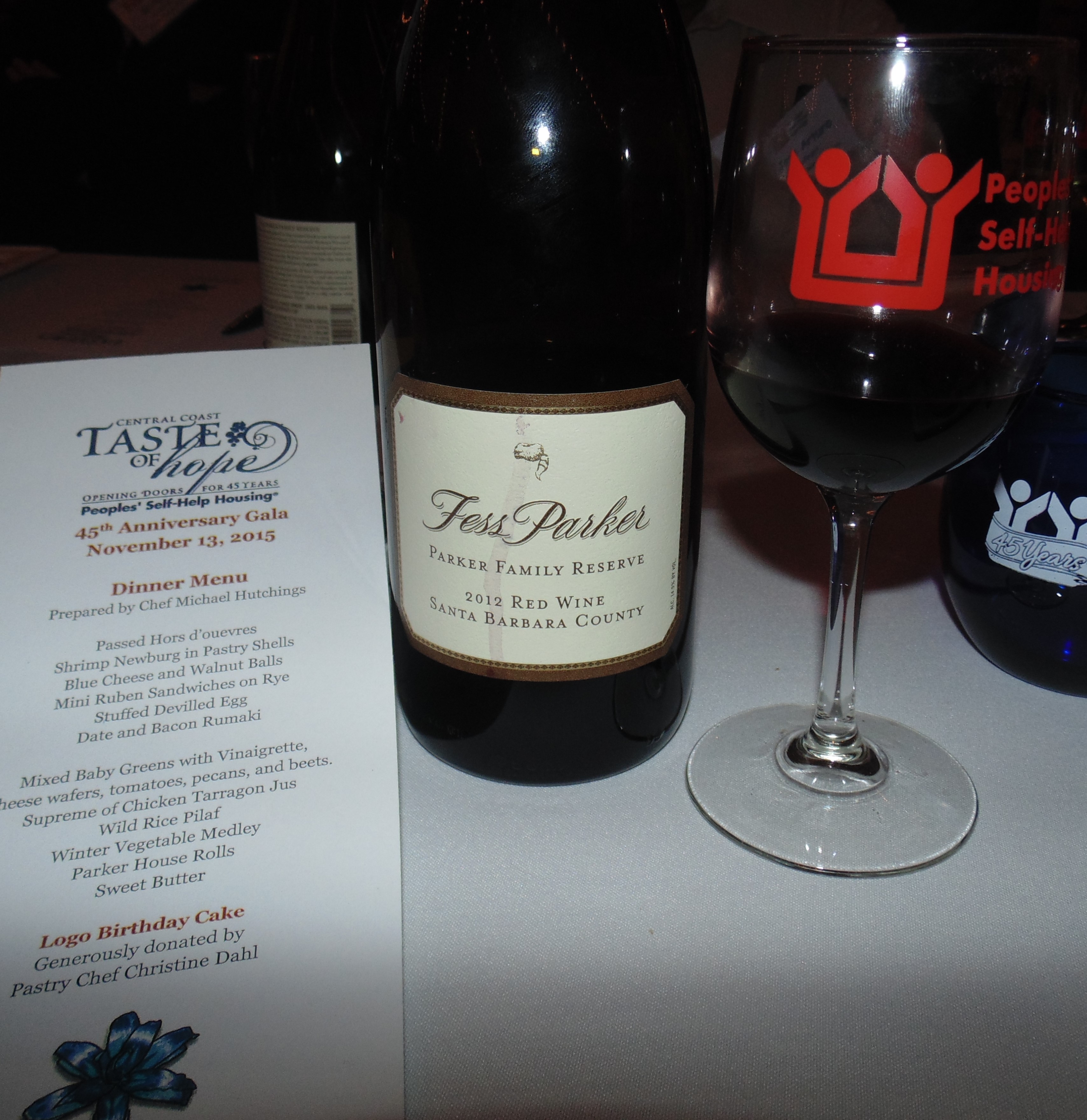  
Founded in 1970, People' Self-Help Housing is an award winning non-profit organization that develops affordable housing and community facilities for low-income households and homeownership opportunities for working families and special needs populations such as seniors. For info visit www.pshhc.org. .jpg)
__________________________________________________ Health Minded .jpg)
Cedars-Sinai Designing ‘Operating Room of the Future’ to Streamline, Improve Trauma CareMedical Center Partners With US Military to Reconfigure Surgical Suites and Adjust Technology to Better Serve Patients With Life-Threatening Injuries Cedars-Sinai has partnered with the U.S. military to design the “operating room of the future” that will enable emergency medical teams to respond more quickly and effectively to patients with life-threatening injuries. Under the project, called “OR 360,” research teams have reconfigured the operating room with movable walls and equipment for more flexible use, identified ways to eliminate disruptions during surgery, and developed an iPhone app that provides diagnostic information about blood pressure and other vital signs before patients arrive in the emergency room. The initiative, drawing on practices from surgery, psychology, aviation and other disciplines, focuses on addressing potential breakdowns in the coordination of trauma care during the so-called “golden hour,” when prompt medical attention can mean the difference between life and death. “Our goal is to improve the efficiency and effectiveness of acute trauma care in both civilian and military settings by introducing innovations in communication, technology, workflows and the way medical personnel perform their jobs,” said Bruce L. Gewertz, MD, surgeon-in-chief and chair of the Department of Surgery at Cedars-Sinai, who also holds the Harriet and Steven Nichols Distinguished Chair in Surgery. “The quicker we get patients cared for, the better the outcomes.” Physicians from Cedars-Sinai and military hospitals on two continents, along with researchers from several universities, have analyzed the complex processes of trauma care – from the moment a doctor’s pager is triggered to the time a patient arrives in a trauma bay to the patient's transfer to an intensive care unit. The aim of this research has been to find ways to simplify the time-pressured nature of trauma care. Gewertz said that means improving communication and teamwork among medical staff, making better use of technology and re-engineering the operating room so that bulky equipment pivots effortlessly around surgical teams rather than cluttering work spaces. OR 360 has been funded by $3.8 million in grants from the U.S. Department of Defense. Cedars-Sinai has collaborated with personnel at military medical centers in the United States and Europe. Important partners in these efforts have included faculty members from the University of Washington, University of Wisconsin-Madison and University of Central Florida. Private sector representatives have come from Coolfire Solutions, a mobile application developer in St. Louis; and the Surgical Safety Institute, a consulting firm in Tampa, Fla., that applies aviation safety techniques to the operating room. Members of this wide-ranging team have based their work on “human factors” research to evaluate the interplay of teamwork and technology, as well as operating room culture and workspaces, among other things. This analysis has zeroed in on “surgical flow disruptions” – such as missing equipment, tangled IV tubes, extraneous conversations and delays in getting specialists or interpreters to the operating room – that can interrupt or slow the work of surgical teams. A broad body of research has found a direct link between flow disruptions in the operating room and surgical errors. To learn how military hospitals avoid these types of disruptions, members of the Cedars-Sinai team visited military surgical teams in the U.S. and Europe to observe their practices and to interview surgeons, nurses and other medical personnel. Team members took away important lessons about standardizing the setup of trauma bays and how to better use technology in the operating room. As an outgrowth of the visits and subsequent research, Cedars-Sinai has introduced several of its own innovations to streamline trauma care, including: - Creating color-coded trauma bays, allowing staffers to more quickly locate supplies and equipment.
- Installing whiteboards in trauma bays that display key patient information such age, gender, pre-hospital vital signs and field treatment, providing important facts as trauma teams respond to fluid situations.
- Developing an iPhone application that puts patient diagnostic data at the fingertips of surgeons, nurses, pharmacists and other trauma team members as they converge on a case from different parts of the medical center.
- Conducting pre-briefings in trauma bays before trauma patients arrive, allowing doctors, nurses and others to understand their roles and to ensure that correct equipment and medications are ready.
These changes have produced promising early results. The whiteboards and pre-briefings, for example, reduced the time to capture first radiological images by more than 10 percent and the time to draw blood for first lab tests by more than 20 percent. The standardized, color-coded trauma bays reduced the time needed to collect supplies by about 15 percent. Cedars-Sinai researchers also are evaluating ways to reduce delays and errors during “hand-offs,” when patients are transferred from one medical space to another (for example, from the operating room to the intensive care unit). And they have designed and built a simulated operating room that features flexible, moving walls and pieces of equipment attached to ceiling tracks that pivot around surgical teams. The lab fosters creative solutions to complex logistical challenges in the operating room. “This is a new way to think about the improvement and delivery of healthcare,” Ken Catchpole, PhD, director of Surgical Safety and Human Factors Research at Cedars-Sinai, said of the overall project. “It’s not just about new techniques or technologies or drugs, but how all those things work in unison. By putting the patients and clinicians at the center of the system, and designing everything directly for their needs, we can develop trauma care for the 21st century that is fast, efficient, safe and of the highest quality possible.” The initiative was supported by a contract that was awarded by the U.S. Army Medical Research and Materiel Command and managed by the Telemedicine & Advanced Technology Research Center (TATRC) under Award Nos. W81XWH1011039 and W81XWH1110813. The views, opinions and/or findings contained in this new release are those of the author(s) and should not be construed as an official Department of the Army position, policy or decision unless so designated by other documentation.
|





